Vulva cancer is a rare form of cancer that affects the outer part of a woman’s genital organs. Though uncommon, it is a serious condition that can significantly impact a woman’s health and quality of life. Early detection and appropriate treatment are crucial for positive outcomes. In this article, Dr. Saurabh Phadnis, a renowned expert in London, provides in-depth insights into the causes, diagnosis, and potential complications of vulva cancer.

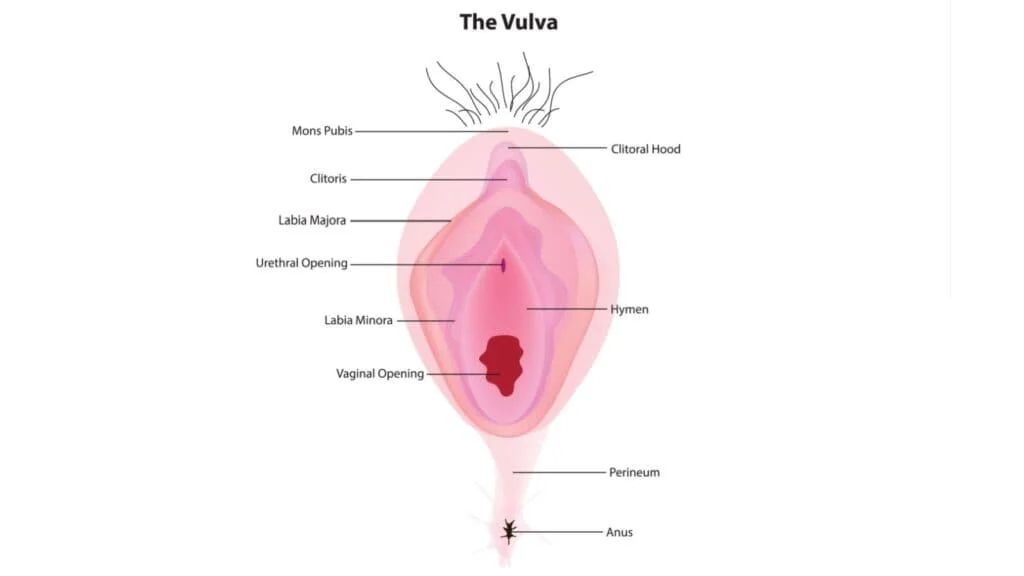
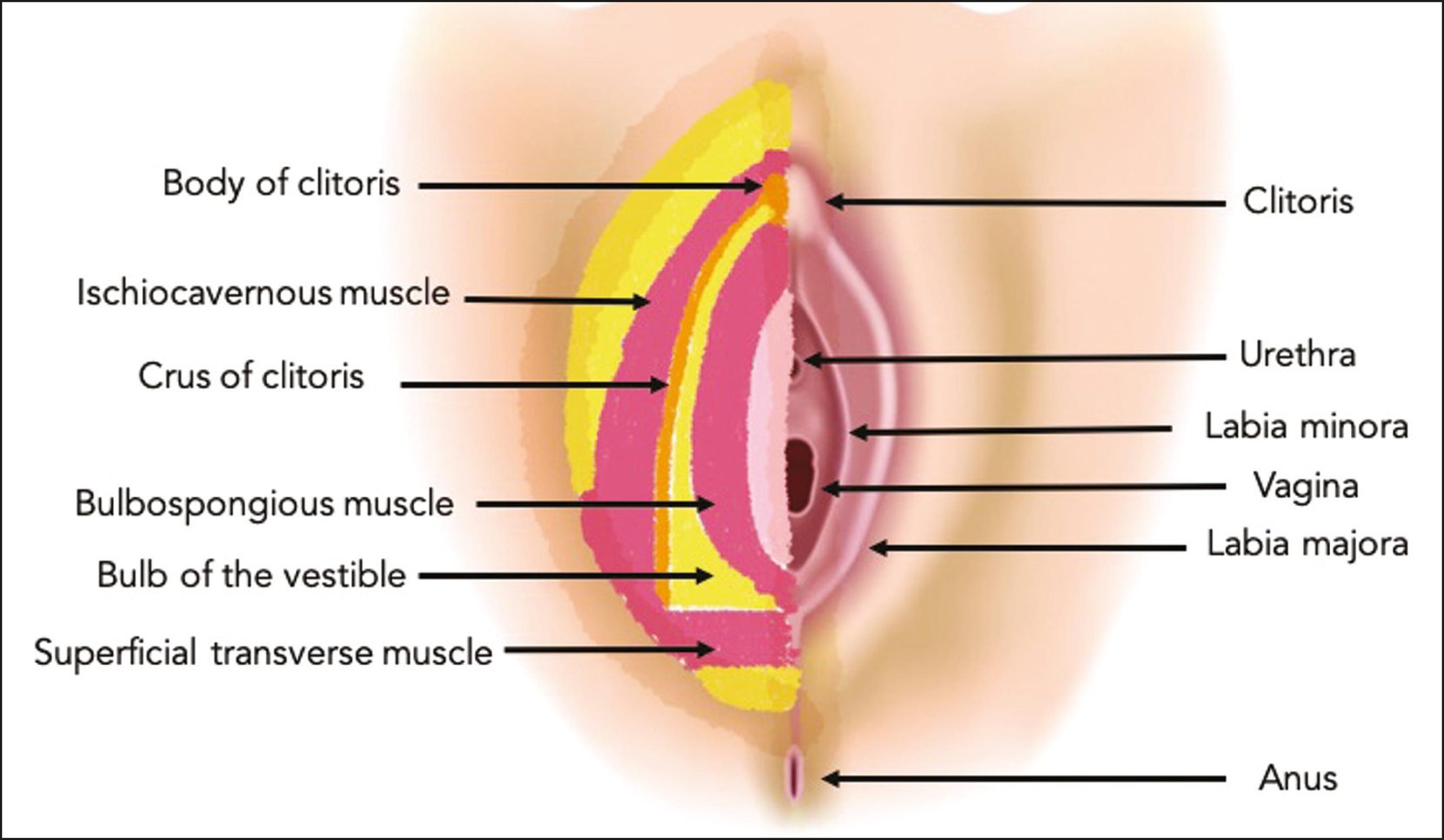
Vulva cancer is a type of cancer that develops in the external female genitalia, known as the vulva cancer. It can affect the labia, clitoris, and vaginal opening.
The most common form of vulva cancer is squamous cell carcinoma, but there are other rare types, such as melanoma and basal cell carcinoma, which are important to recognise as part of gynaecological cancer awareness and management.
The following causes and risk factors may contribute to the condition:
A major contributor to vulva cancer, particularly types 16 and 18 of HPV.
Most cases of vulva cancer occur in women over the age of 60.
Individuals with weakened immune systems, are more susceptible to developing vulva cancer.
Chronic conditions like lichen sclerosus, can increase the risk of vulva cancer.
Smoking is a well-known risk factor for many cancers, including vulva cancer.
Women should remain vigilant and consult a healthcare professional if any of the following symptoms occur:
Persistent itching or burning in the vulvar area that does not go away with topical treatments.
Lumps or growths in the vulva that may be hard, raised, or ulcerated. These could be signs of a developing tumour.
Pain during sexual intercourse or while sitting may be caused by abnormal growths.
Unexplained bleeding, particularly after intercourse, or unusual discharge from the vulva.
Skin on the vulva may change in appearance, becoming thicker, discolored, or forming ulcers.
Several diagnostic steps are used to confirm the presence of vulva cancer:

A personalised treatment plan will be developed to provide the best possible outcomes for each patient.
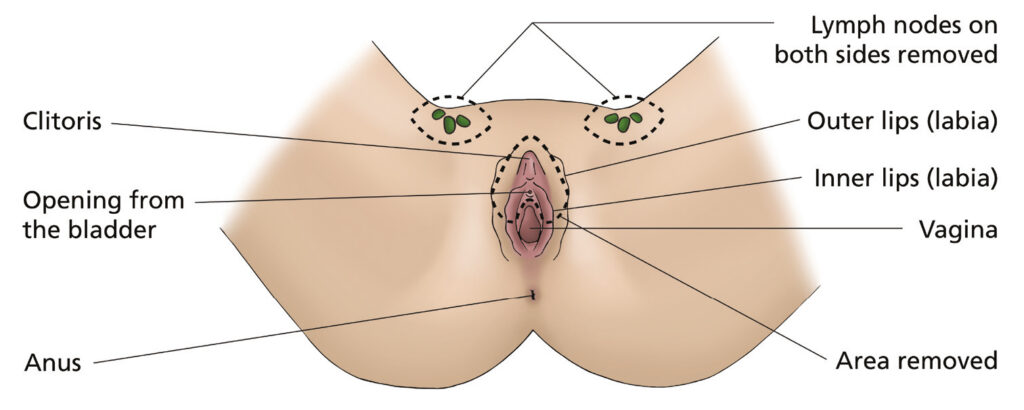
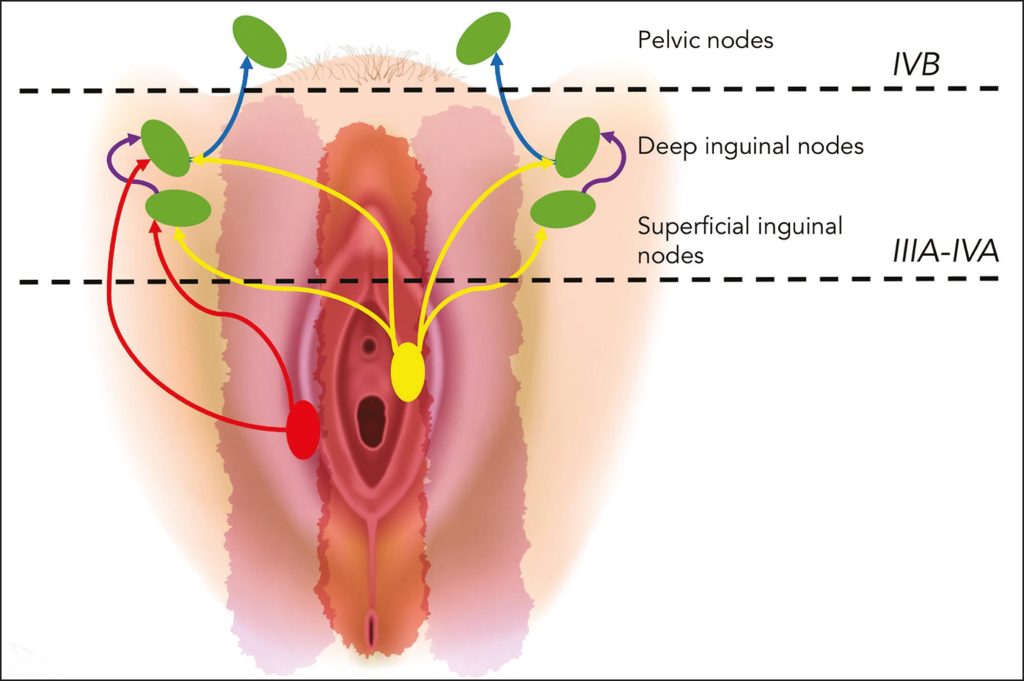
Surgery is the most common treatment for vulva cancer.
Radiation therapy is often used in conjunction with surgery to kill any remaining cancer cells.
Chemotherapy may be recommended if the cancer has spread to other parts of the body.
These newer treatments focus on attacking specific cancer cells or boosting the body’s immune response to cancer.
In advanced cases, palliative care is provided to manage symptoms and improve the quality of life for patients.
Vaccinating against HPV can help prevent the infection that leads to vulva cancer.
Regular gynaecological exams can help detect abnormalities early.
Avoiding smoking, maintaining a healthy immune system, and managing chronic conditions can reduce the risk of vulva cancer.
If you have conditions like lichen sclerosus, regular monitoring and treatment can help reduce the risk of developing vulva cancer.

Vulva cancer is a rare but serious condition that affects many women. With early detection, proper treatment including procedures such as pelvic lymph node excision and lifestyle changes, the chances of overcoming the condition are significantly improved.
If you notice any symptoms or are at higher risk, it is crucial to consult a healthcare provider for an early diagnosis.
Dr. Saurabh Phadnis offers expert care for vulva cancer patients in London, guiding you through every step of the process from diagnosis to recovery.
If you’re concerned about Vulva cancer, private consultations are available with Dr. Saurabh Phadnis, leading Gynaecologist, Oncologist, Surgeon, and Co-Lead Colposcopist based in London; specialising in gynaecological cancer. You can visit his clinic or call directly to book an appointment and receive expert care, advice, and personalised treatment.
While vulva cancer cannot be fully prevented, getting the HPV vaccine and maintaining regular gynaecological check-ups can significantly reduce your risk.
Survival rates depend on the stage at which vulva cancer is diagnosed. Early-stage vulva cancer has a higher survival rate, while advanced stages may require more intensive treatment.
If you notice persistent itching, lumps, ulcers, abnormal bleeding, or other unusual changes in the vulva, it’s important to consult a healthcare provider for a thorough examination and diagnosis.
Vulva cancer can cause pain or discomfort, especially if it leads to visible lumps or sores in the genital area. Early treatment can help manage pain and other symptoms.
Recovery time depends on the type and extent of the treatment. After surgery, patients may need a few weeks to recover, while radiation or chemotherapy treatments may require several months.
Specialising in the field of gynaecological cancer, covering the entire spectrum from diagnosis to treatment and post-treatment care.