The national cervical screening programme represents one of the most significant triumphs in modern preventative medicine, a proactive measure designed to protect health and offer peace of mind. Yet, for the individual who receives a letter stating their recent smear test has yielded an ‘abnormal’ result, it can feel anything but peaceful. This single word can trigger a cascade of concern, casting a shadow of uncertainty. It is in these moments that expert, empathetic guidance becomes paramount.
In London, Mr Saurabh Phadnis, a leading Consultant Oncological Surgeon with deep expertise as a Robotic Surgeon, Colposcopist, and Gynaecologist, provides that essential clarity. He emphasizes that this result is not an endpoint but a signpost on a well-defined path. It signals that the screening process is working effectively, identifying cellular changes at a stage where they can be managed simply and successfully, turning a moment of anxiety into an opportunity for empowered health management.
Receiving a notification of an abnormal result is the first step in a dialogue about your cervical health. The terminology used, such as ‘dyskaryosis’, can seem intimidating, but it is simply the medical term for changes in the cells on the surface of the cervix. It is vital to understand that these changes are not cancer. They are graded on a spectrum, from borderline or mild changes to moderate or severe. This grading system provides a detailed picture of the cellular activity, allowing specialists to determine the most appropriate and proportionate response. The screening test has successfully done its job by flagging these changes early, initiating a process of careful assessment and management. This early detection is the key to prevention, ensuring that any potential issues are addressed long before they could pose a significant threat to your health, a cornerstone of the care provided by specialists like Mr Phadnis.
Modern cervical screening in the UK now tests for high-risk types of the Human Papillomavirus (HPV) first. This is because persistent infection with HPV is responsible for almost all cases of cervical cell changes and, eventually, cervical cancer. Finding HPV in your sample is very common; most adults will encounter the virus during their lifetime, and in the vast majority of cases, the immune system clears it without any issue. An HPV-positive result simply means the virus is present, which is why the sample is then checked for any cell changes (cytology). It is a highly sensitive approach that allows for more accurate risk assessment. It is crucial to remember that having HPV is not a reflection on your lifestyle or fidelity and does not impact your ability to have a family. It is simply a common virus that requires diligent monitoring through the established screening pathway.
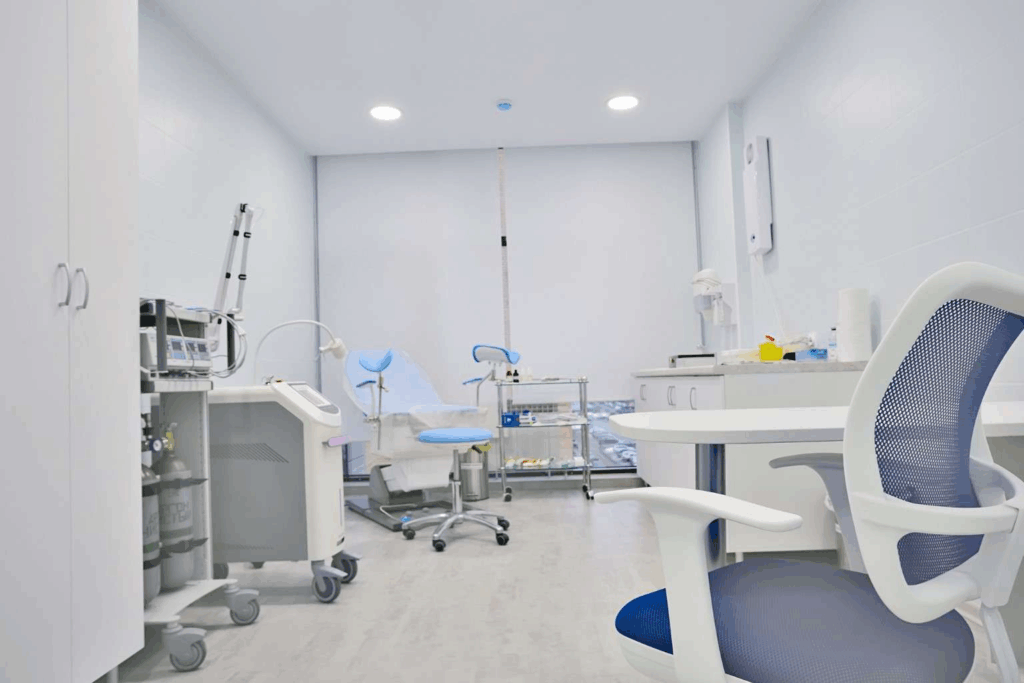
If your screening result shows both an HPV infection and abnormal cell changes, you will be referred for a colposcopy. This is a diagnostic procedure, not a surgical one, and it allows a specialist to get a much clearer look at your cervix. The appointment itself feels very much like having a smear test and is conducted in a hospital or clinic setting. A speculum is gently inserted, and the colposcopist uses a large, illuminated magnifying device—the colposcope—to examine the cervical tissue in detail. The instrument remains outside your body, acting like a pair of binoculars. To highlight any areas of abnormal cells, a special liquid is painted onto the cervix. This might cause a brief, mild stinging or tingling sensation but is not painful. The entire examination is a well-tolerated and essential step in gaining a comprehensive understanding of your cervical health.
During the colposcopy, the specialist may see areas that require further investigation. In such cases, a small tissue sample, or biopsy, is taken. This is a very quick process, often described as a sharp pinch, and it provides a wealth of information. The sample is sent to a laboratory where a pathologist can confirm the exact grade of the cell changes, known as Cervical Intraepithelial Neoplasia (CIN). CIN is graded from 1 to 3, corresponding to how much of the cervical lining is affected by the abnormal cells. CIN 1 represents very mild changes that often resolve on their own, while CIN 2 and 3 indicate more significant changes that typically require treatment. The biopsy result is the definitive piece of the puzzle, allowing your consultant to create a precise and personalised management plan that is perfectly suited to your clinical needs.
A result of CIN 1 indicates that only the surface layer of the cervix has mild cell changes. This is the lowest grade of abnormality and is considered to have a very high chance of regressing spontaneously. The body’s immune system is often powerful enough to clear the underlying HPV infection, which in turn allows the cervical cells to revert to normal without any medical intervention. For this reason, the standard approach for CIN 1 is active monitoring rather than immediate treatment. This usually involves a follow-up cervical screening test in twelve months’ time to ensure the cells are returning to normal. This patient and measured approach avoids overtreatment while still keeping a careful, protective watch over your health, ensuring that any persistence of the abnormality is identified and can be acted upon if necessary, balancing vigilance with a conservative methodology.
When a biopsy confirms the presence of CIN 2 (moderate changes) or CIN 3 (severe changes), treatment is generally recommended. It is essential to reiterate that even CIN 3 is not cancer. It is a high-grade precancerous condition, meaning the cells have the potential to become cancerous if left untreated over a period of several years. The recommendation for treatment is a preventative measure designed to remove these abnormal cells and eliminate that future risk. The decision to treat is a proactive and highly effective step. The slow progression of these cellular changes means there is ample time for this intervention to be successful. This is the very purpose of the screening programme—to catch these changes at a stage where a simple procedure can prevent a much more serious diagnosis down the line, a principle that underpins the entire approach to modern gynaecological care.
The most common treatment for high-grade cervical cell changes is the Large Loop Excision of the Transformation Zone, or LLETZ. This is a minor procedure, usually performed under local anaesthetic in the colposcopy clinic itself. The local anaesthetic numbs the cervix, ensuring the process is as comfortable as possible. Using a fine wire loop with a gentle electrical current, the specialist carefully removes the small area of the cervix containing the abnormal cells. The procedure is quick, typically taking no more than 10-15 minutes. The removed tissue is sent for analysis to confirm that all the abnormal cells have been excised. The LLETZ procedure has an exceptionally high success rate and is the definitive step in preventing the progression to cancer, providing both treatment and profound peace of mind in a single, straightforward session.
Following treatment, you can expect a swift return to your normal daily activities, with perhaps some minor, temporary side effects like light bleeding or discharge. Importantly, the treatment does not affect your long-term health, your fertility, or your ability to enjoy a full and active life. The most critical part of the post-treatment journey is attending your follow-up appointment, which is usually scheduled for six months later. This appointment, a test of cure, involves a smear test to check for the presence of HPV. A negative result confirms the treatment was successful and that your immune system has cleared the virus. You will then return to the routine screening schedule. Adherence to this follow-up is the single most important action you can take to ensure your continued cervical health and the long-term success of your treatment.
Navigating the path from an abnormal smear result to a clean bill of health is a journey of partnership between you and your healthcare team. It is a process built on clear communication, advanced diagnostics, and effective, preventative treatment. An abnormal result is not a cause for despair but a call to action—an opportunity to engage proactively with your health under the guidance of a dedicated specialist. The UK’s cervical screening programme is a world-class system designed to protect you, and every step, from the initial letter to the final follow-up, is a carefully considered part of that protective shield.
For those in London seeking the highest level of expertise and a reassuring, patient-focused approach, a consultation with Mr Saurabh Phadnis offers the clarity and care needed. We encourage you to book an appointment to discuss your results and map out your path to continued health and wellbeing.
The HPV virus can lie dormant in the body for many years before becoming active, or you may have been exposed to it since your last test. A normal result in the past does not guarantee a normal result in the future, which is why regular screening every three to five years is so essential for monitoring your cervical health over time.
HPV is a very common virus that is easily passed between partners through sexual contact. If you have HPV, it is highly likely your partner has also been exposed to it. There is no routine test for HPV in men, and it rarely causes them any health problems. The focus remains on cervical screening for women and individuals with a cervix to prevent cancer.
No. Treatment for abnormal cervical cells, such as LLETZ, is typically a one-off procedure that is highly successful in removing the abnormal cells completely. Once you have a successful ‘test of cure’ result six months after your procedure, you will simply return to the standard national screening programme for routine follow-up.
LLETZ is the most common and widely recommended treatment, but other options exist, such as a cone biopsy, which removes a larger, cone-shaped piece of tissue. The choice of treatment depends on the specific clinical circumstances, including the grade and location of the abnormal cells. Your consultant will discuss the most appropriate option for you.
While there is no medical cure for the HPV virus itself, a strong immune system is your best defence. Leading a healthy lifestyle with a balanced diet, regular exercise, and not smoking can support your immune function. For some, certain supplements may help, but the most important action is to attend all your screening and follow-up appointments as advised.